Visit:
https://cdphe.colorado.gov/colorado-suicide-statistics
Click Suidice Deaths 2004-2019 Bridged (single)races with Hispanic origin.
*Then select: Circumstances, Toxicology, and Injury Location 2020- 2022
*Select: 10-014, 15-18, 19-24 for all races
*Select: Black/African America
And Select: White Hispanic
Early onset marijuana use and suicidal ideation among African American college students, 2023, August 2
Association Between Marijuana Laws and Suicide Among 12- to 25-Year-Olds in the Unit– MML and RML were associated with increased suicide-related mortality in female youth and 14- to 16-year-old individuals of both sexes. 2023, June 26
Suicidality risk after using cannabis and cannabinoids., 2023, June 25
2023, June 25 Suicidality risk after using cannabis and cannabinoids: An umbrella review -Cannabis use was associated with a higher rate of suicidal ideation and attempts in various populations, including BD and MDD patients, military veterans, and the general population. Evidence for a causal relationship was mentioned in one study for suicidal ideation.
Cannabis Use Is Associated With Depression Severity and Suicidality in the National Comorbidity, 2023, March 2
US trends in the association of suicide ideation/behaviors with marijuana use among adolescents ages 12-17, January 2023
Does marijuana use lead to suicidal tendencies in some adolescents?
Yes. Two independent studies came up with a very similar elevation in risk (nearly 7-fold):
https://www.thelancet.com/journals/lanpsy/article/PIIS2215-0366(14)70307-4/fulltext
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4219077/pdf/wps0013-0322.pdf
Part of the risk for suicide may be exerted through the mental disorders that marijuana triggers (as
referenced previously), particularly psychotic disorders and depression:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4197787/pdf/cjp-2014-vol59-october-531-538.pdf
However, there is also evidence that marijuana’s effect can be more immediate from a recent study
illustrating the likelihood of suicidal thoughts increased on the days when an adolescent uses
marijuana:
https://www.sciencedirect.com/science/article/abs/pii/S0165178118323321?via%3Dihub
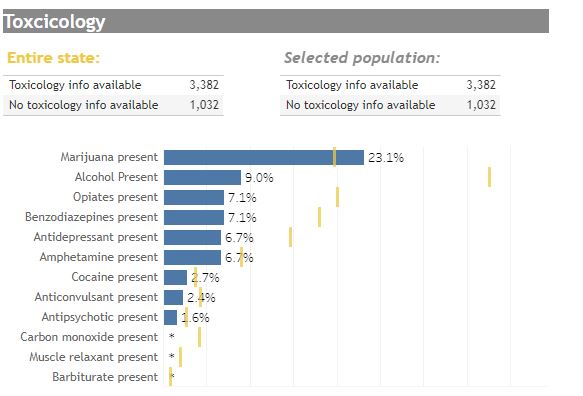
In Colorado, the THC positive toxicology screens in youth aged 15-19 have consistently increased
over the past several years (while such data was being collected by the Colorado Department of
Health), such that it became the leading drug found in suicide victims of that age range (32% were
positive by 2017, about 1.5-fold higher than the average monthly use rate for that age group in
Colorado):
https://cohealthviz.dphe.state.co.us/t/HSEBPublic/views/CoVDRS_12_1_17/Story1?:embed=y&:sho
wAppBanner=false&:showShareOptions=true&:display_count=no&:showVizHome=no#4
Colorado has experienced an overall year-to-year increase in teen suicides:
https://www.cpr.org/2019/09/17/the-rate-of-teen-suicide-in-colorado-increased-by-58-percent-in3-years-making-it-the-cause-of-1-in-5-adolescent-deaths/
Although the rate of teen use has not increased that much in Colorado, the potency of what is used
by youth in states with legalized marijuana has increased markedly:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5534375/pdf/nihms880035.pdf
Select: https://cohealthviz.dphe.state.co.us/t/HSEBPublic/views/CoVDRS_12_1_17/Story1?%3Aembed=y&%3AshowAppBanner=false&%3AshowShareOptions=true&%3Adisplay_count=no&%3AshowVizHome=no#4
1. Circumstances, Toxicology, and Injury location
2. Select the year slide from 2014 to present
3. Age (drop box): check only 10-14 and/or 15-18.
Association of suicidality trends with cannabis use…
- From 2008 to 2019, suicidal ideation, plan, and attempt increased 40% to 60% over increases ascribed to cannabis use and MDE (major depressive episode).
- Non-daily users, daily users, and those with CUD (cannabis use disorder), were associated with a higher prevalence of suicidal ideation, plan, and attempt more significantly in women than in men.
- Because the prevalence of CUD increases with time since initiation of use among young adults (18 to 34 years old), the results of the paper underscore an urgent need for prevention interventions designed specifically for young people before first cannabis exposure and highlight the importance of early screening for daily cannabis use and CUD, as well as, CUD treatment, especially among young women.
- Hahn B, et al. Associations of suicidality trends with cannabis use as a function of sex and depression status. JAMA Network Open. 2021 Jun; 4(6): e2113025. Published online 2021 Jun 22.
https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2781215
Association of Cannabis Use With Self-harm and Mortality Risk Among Youths With Mood Disorders
Conclusions and Relevance Cannabis use disorder is a common comorbidity and risk marker for self-harm, all-cause mortality, and death by unintentional overdose and homicide among youths with mood disorders. These findings should be considered as states contemplate legalizing medical and recreational marijuana, both of which are associated with increased CUD.
https://jamanetwork.com/journals/jamapediatrics/fullarticle/2775255
Cannabis use may be associated with suicidality in young adults
An analysis of survey data from more than 280,000 young adults ages 18-35 showed that cannabis (marijuana) use was associated with increased risks of thoughts of suicide (suicidal ideation), suicide plan, and suicide attempt. These associations remained regardless of whether someone was also experiencing depression, and the risks were greater for women than for men. The study published online today in JAMA Network Open and was conducted by researchers at the National Institute on Drug Abuse (NIDA), part of the National Institutes of Health.
Applying the Bradford Hill Criteria for Causation to the Relationship
Between Marijuana Use and Suicidal Behavior
Christine L. Miller, Ph.D.
September 2020
In 1965, Sir Bradford Hill developed a set of tests designed to elucidate causal relationships in epidemiology. These criteria have subsequently become accepted as important standards for epidemiological and clinical science, as reviewed by van Reekum et al. (2001) for neuropsychiatry applications.
1) Demonstration of a strong association between the causative agent and the outcome (author’s note: often termed “correlation”, it is the first criteria required to be satisfied for causation): √
Among the largest effect sizes for increased risk of suicide attempt in marijuana users were found in two longitudinal studies of predominantly Caucasian youth, both of which adjusted for a variety of potentially confounding factors. One study combined 3 longitudinal data sets involving 6 to 9 assessments over a period of 15 years, finding a 6.9-fold increase in risk for subsequent suicide attempt in those using marijuana daily before age 17 (Silins et al., 2014). As well as adjusting for measures of depression and conduct disorder, along with a variety of demographics, the adjustment factors specific to other drug use included tobacco use, alcohol use and other illicit drug use. The second longitudinal study with a large effect size included two assessments and a follow-up time of 8 years (Clarke et al., 2014), and was notable in that it adjusted for a history of any mood disorder (including depression), in addition to familial/adolescent risk factors, alcohol use but not tobacco or other drug use, finding a 7.5-fold increase in risk for suicide attempt when the marijuana use commenced in the teen years. As the best predictor of completed suicide is suicide attempt (Nordstrom et al., 1995; Hawton et al., 2013), it would be expected that the increased risk would be fairly similar in magnitude for suicide attempt and completed suicides. Indeed, a 2013 study of predominantly Caucasian subjects found a 5.3-fold increased risk for completed suicide in those with a cannabis use disorder (Arendt et al., 2013). Although a variety of demographic and personal risk factors were adjusted for, other substance use was only available for the month before cannabis abuse treatment commenced.
2) Consistency of the findings across research sites and methodologies: √
A meta-analysis of a mix of longitudinal and case-control studies worldwide, some including a mix of ethnic groups (African ancestry, Hispanic ancestry) with a lower risk of suicide than Caucasians (Curtin et al., 2016), found an overall 2.2-fold increase in risk for suicide attempt in users of marijuana, a 3.2-fold increased risk of suicide attempt in heavy users, and a 2.6-fold increase in risk for completed suicides in ever users (Borges et al., 2016). The follow-up times in the longitudinal studies ranged from 1 year to 33 years, averaging somewhat less than 7 years. There have been only a few reports that failed to find an association, including a case-control (no follow-up) study of 9,268 Swiss adolescents (Gex et al., 1998). Given the study size, the lack of follow-up limited the sensitivity of the study, and the investigators found no association between suicide attempt and marijuana use after controlling for a variety of potentially confounding variables, including tobacco smoking. Because very many marijuana users during that general time period also began smoking tobacco if they were not already smokers (Patton et al, 2005), correcting for tobacco use would be expected to substantially reduce the effect size of marijuana and therefore, could potentially explain the lack of association found depending on the study power. In a study of other mental health outcomes in 50087 Swedish conscripts by Zammit et al. (2002), 86% of the marijuana users also smoked cigarettes. In the same cohort, Price (2009) found that an unadjusted 1.6-fold increase in risk for completed suicide in the 33-year longitudinal study was eliminated after adjusting for confounding variables, including smoking of tobacco. Although the total study population was quite large, the small number of completed suicides expected in the cannabis-using group (likely <30), means statistical power may have been quite limited after adjustments for confounding variables. Suicide attempts are much more frequent and afford greater statistical power. A longitudinal study of suicide attempts by Rasic et al. (2013) in a cohort of 976 Canadian high school students over a two year period, found that marijuana users were more likely to be depressed after adjusting for other illicit drug use and alcohol (but apparently not tobacco), but were not significantly more likely to attempt suicide than nonusers. Notably, this study was underpowered to detect anything less than a 2.7-fold effect of marijuana on suicide attempt (a smaller increase in risk would certainly be of interest, particularly since the two year follow-up period was so short). The evidence for tobacco use confounding the association of marijuana with suicide risk is strong (Miller et al., 2011; Bohnert et al., 2014; Evins et al., 2017). Yet, after decades of tobacco prevention education, the use of tobacco by U.S. youth began to decline (Centers for Disease Control, 2020), as well as use by all age groups worldwide (WHO, 2019) while marijuana-only use has increased (Schauer and Peters, 2018) to the extent that it became easier for researchers to investigate marijuana-specific effects independent of cigarette use. In a recent case-control study (Kahn and Wilcox, 2020) of a large (59,079) ethnically mixed population of U.S. high school students, adjusting for a variety of factors as well as tobacco and alcohol use revealed that the impact of marijuana on suicide attempts was still significant, with an enhanced prevalence of suicide attempt of 2.6-fold for those who used marijuana 20 or more days per month and at that same rate of use, a 4.5-fold enhanced prevalence of suicide attempts requiring medical intervention. There was no follow-up in this study of incident marijuana use and suicidal behaviors over one year, and for the studies reviewed by Borges et al. (2016), the follow-up was on average shorter than the Silins et al. and Clarke et al. studies mentioned above showing higher impact. Kahn et al. also reported that marijuana use was generally equivalent to the impacts of tobacco and alcohol; however, this proportionality might not persist in a longitudinal study because the relative impact of each substance could theoretically change as more suicide attempters are registered over time in a cohort population.
3) Demonstration of specificity of the causative agent in terms of the outcomes it produces: N/A (see van Reekum et al., 2001)
This criterion may be applicable to outcomes from infectious organisms to a certain extent, but is considered not considered applicable to neuropsychiatry and neuropharmacology (van Reekum et al., 2001), where one drug can result in many different outcomes and conversely, many different drugs are associated with suicidal behavior, including tobacco products, alcohol (Kahn and Wilcox, 2020) and other recreational drugs of abuse (reviewed by Miller, 2018).
4) Demonstration of the appropriate temporal sequence so that the causative agent occurs prior to the outcome: +/-
More work needs to be done on the timing of marijuana use and suicide, although the existing data is strongly suggestive of an appropriate temporal sequence in some, but not all, studies. For this criterion, longitudinal studies are the most important. Of those identified with adequate assessment intervals and time frame, one (also described above) involved the analysis of 3 separate longitudinal studies combined, totaling 2675 predominantly Caucasian youth starting at age 16 for each study, with follow-up through age 30, as reported by Silins et al. (2014). Yearly assessments were conducted (with mental health data prior to age 16 acquired retrospectively), numerous potentially confounding variables were adjusted for, and for those youth who were using marijuana daily by the age of 17, the risk of suicide attempt over the ensuing years was found to be significantly increased (6.9-fold) as compared to controls. A subsequent meta-analysis of only longitudinal studies assessing marijuana use that commenced at ages less than 18 years (Gobbi et al., 2019), identified a significant 3.46-fold increase in risk for suicide attempt during young adulthood in those with no pre-existing suicidal behaviors, depression or anxiety. Not all of the included studies adjusted for other drugs of abuse, use of tobacco cigarettes, or psychosocial factors. A third longitudinal analysis found no significant impact of marijuana on suicide attempt (Agrawal et al., 2017), utilizing a database that assessed an ethnically mixed group of 3277 subjects (30% African American, 70% Caucasian) every two years over a period of 10 years, and encompassed a large age range at study inception, ages 12 to 22. Even early marijuana use (<15 yrs of age) was not significantly associated with subsequent suicide attempt; however, the study was underpowered to detect less than a 1.5-fold increase in risk. Intriguingly, a prior history of suicidal ideation was significantly protective for initiating marijuana use, while prior suicide attempts had no impact on initiating marijuana, though lack of statistical power would have influenced the latter result. Unlike the Silins et al. study, they did not investigate the effect of frequency of use on later suicide attempts. The study adjusted for race, but did not report a separate analysis for Caucasians alone. Yet, a recent data summary of case reports, with no statistical analysis, found that for 303 adults (aged 18 and over) with a self-reported history of marijuana use admitted over a 4 month period to the Emergency Department of an urban hospital, (Marco et al., 2020), 9% had experienced suicidal ideation in the past 30 days (whereas 2.4% has been reported as the one month prevalence in the adult population by Olfson et al., 1998, and 4.6% as the one month prevalence for teens, Turner et al., 2012), and most strikingly, of the 41% who had experienced lifetime suicidal ideation, the timing of their marijuana initiation preceded the onset of suicidal ideation in the vast majority of cases (91%). Of note, the majority did not perceive any harm associated with their use and therefore, were not attempting to excuse mental health problems by revealing marijuana use. Suicidal ideation, however, is not as strong a predictor of subsequent suicide as is a suicide attempt (McHugh et al., 2019; Nordstrom et al., 1995; Hawton et al., 2013). No statistical analysis nor correction for potentially confounding variables was carried out. The subjects were a fairly balanced mix of Caucasians and African Americans, with a small percentage of Hispanics and other groups. Rather than limiting the analysis to a direct effect of marijuana use on subsequent suicidal behavior, the effect of marijuana to trigger mental health disorders (major depression, bipolar disorder and schizophrenia; Miller, 2018) must be evaluated as an indirect mechanism leading to risk for suicide, because such disorders are associated with a much greater risk (7 to 21-fold) during the early stages of illness, even in the absence of marijuana use (Randall et al, 2014). Nussbaum et al. (2011) published a case report concerning a patient whose depression surfaced after marijuana use began at age 18, eventually leading to polydrug use. In the weeks before the patient’s suicide attempt, it was her marijuana use that doubled. For such indirect cases, the temporal sequence would nevertheless be satisfied. Finally, there is some evidence that marijuana can exert an acute effect to increase suicide risk in the short term, where the temporal sequence is more clear. In such cases, the acute effect of marijuana may be more similar to alcohol (Kaplan et al., 2013) than to tobacco (Kassel et al., 2007). Although rates of lifetime suicidal ideation or suicide attempts can be surprisingly high (e.g. Agrawal et al., 2017) , the acute risk on any particular day for the general population remains very low; therefore, reports of a temporal sequence of events over a few days or on the same day, carry more meaning. Among marijuana using teens (68% Caucasian), use of marijuana on a particular day is reported to be a predictor of a suicide attempt on that day (Sellers et al., 2019). Lacking more extensive longitudinal research on the issue, case reports and anecdotal evidence can also offer some important insights. Suicidal ideation was observed in one out of fourteen subjects administered a liquid form of pure ∆9 – THC (20 mg doses) over a period of 3 days in a clinical setting (Gorelick et al., 2011). Russo et al. (2015) observed the onset of suicidal ideation in a patient treating the spasticity of multiple sclerosis with a formulation containing ∆9 – THC. Multiple sclerosis patients are already at higher risk for suicide, and a similar impact of ∆9 – THC has been observed in other cases (Langford et al., 2013). Koppel et al. (2014) review reports of suicidal ideation following medical use of cannabinoids. Episodic marijuana use in a patient was found to result in acute suicidal ideation only during the periods of use (Raja and Azzoni, 2009), with a return to normalcy in the intervals of non-use. A Centers for Disease Control MMWR report attributes the intentional and fatal jump of a young college student from a hotel balcony to his recent consumption of a potent marijuana edible (Centers for Disease Control, July 24, 2015). The anecdotal report of a New York Times columnist (Dowd, 2014) describes overwhelming feelings of impending doom that lasted for hours after consumption of a potent marijuana candy bar during her 2014 visit to Colorado, and such feelings could be expected to lead to suicidal urges in those less able to mentally cope. Following Dowd’s experience, a young, seemingly very well-adjusted college graduate visiting Keystone in 2016 to ski with his cousin, killed himself after consuming too many marijuana edibles, as reported by Michael Roberts in Westword (March 26, 2015). Roberts also covered the selfstabbing death of Daniel Juarez who was intoxicated from high levels of ∆9 – THC in his system and the suicide of Brant Clark, which occurred a few weeks after he experienced a psychotic break from marijuana use (Roberts, May 19, 2015).
5) Demonstration of a biological gradient, in which more of the causative agent leads to a poorer outcome: √
Here, the studies looking at frequency of use show greatest impact with higher use rates (daily use most impactful, inferred from Silins et al., 2014; “heavy use” of greater impact than ever-use in a meta-analysis by Borges et al., 2016). Kahn and Wilcox (2020) provide a more fine-tuned investigation of the impact of frequency of use, investigating marijuana use rates of 1-2, 3-9, 10- 19 and 20+ use days per month, and finding an enhanced prevalence of suicide attempt (as compared to nonusers) of 1.65, 2.11, 2.13 and 2.64-fold respectively. The corresponding figures for suicide attempt requiring medical intervention were 1.98, 2.52, 3.15 and 4.51-fold.
6) Demonstration of a biologic rationale, such that it makes sense that the suspected agent causes the outcome: √
Bloomfield et al. (2016) reviewed the overall experimental evidence that ∆9 – THC stimulates the dopaminergic reward system of the brain, and over time, depletes the integrity of the system leading to exhaustion of dopaminergic tone. As this reward system is important to deriving pleasure from everyday life, it is understandable that chronic use of THC may lead to a loss of interest in continuing to live. Several drugs of abuse act on the dopamine reward system (Blum et al., 2015).
7) Coherence of the findings, such that the causation argument is in agreement with what we already know: √
Suicide causation is almost always multifactorial (Pandey, 2013; Vijayakumar et al., 2016) and rarely associated with a single cause; therefore, this criterion is satisfied as it is consistent with what is known about other suspected causes, i.e. the impact of chronic marijuana use is thought to be exerted primarily in conjunction with other factors.
8) Experimental evidence: √
As stated above: “Suicidal ideation was observed in one out of fourteen subjects administered a liquid form of pure ∆9 – THC (20 mg doses) over a period of 3 days in a clinical setting (Gorelick et al., 2011). Subjects at already higher risk for suicide may similarly show a temporal relationship between suicidal ideation and administration of formulations containing ∆9 – THC (Langford et al., 2013). Koppel et al. (2014) review reports of suicidal ideation following medical use of cannabinoids.”
9) Evidence from analogous conditions: N/A (see van Reekum et al, 2001)
For neuropsychiatric outcomes, parallels between related neuropsychiatric conditions is not a necessary finding because the response of the brain to different insults is so complex.
Conclusions All but one (#4) of the seven relevant Bradford Hill criteria have been satisfied for the causal connection between marijuana use and the development of suicidal behavior. The evidence that an “appropriate temporal sequence” exists (outlined in criterion #4) is strongly suggestive though remains unconfirmed from an academic standpoint. Further study is required in the form of longitudinal studies that are prospective in nature. Adequate length of follow-up time and number of assessment intervals, ability to adjust effectively for poly-substance use with respect to timing of use, distinguishing acute from chronic effects, addressing ethnic diversity with respect to outcome and ensuring adequate statistical power should be incorporated in future research paradigms. Nevertheless, the weight of the evidence currently available should be regarded as strong enough to elicit widespread public health warnings about the suspected role of marijuana use in precipitating suicidal behaviors, since the mandate of the relevant authorities is to err on the side of protecting public health rather than to establish scientific certainty beyond a shadow of a doubt. This is particularly urgent in view of the continuing increase completed suicides in conjunction with rising marijuana use rates and more potent products, not only in specific states but across the nation as a whole (Miller et al., 2020).
References Agrawal A, Nelson EC, Bucholz KK, Tillman R, Grucza RA, Statham DJ, Madden PA, Martin NG, Heath AC, Lynskey MT. Major depressive disorder, suicidal thoughts and behaviours, and cannabis involvement in discordant twins: a retrospective cohort study. Lancet Psychiatry. 2017;4(9):706-714. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5696002/pdf/nihms896582.pdf
Arendt M, Munk-Jørgensen P, Sher L, Jensen SO. Mortality following treatment for cannabis use disorders: predictors and causes. J Subst Abuse Treat. 2013; 44(4):400-406. https://www.journalofsubstanceabusetreatment.com/article/S0740-5472(12)00382-0/fulltext
Bloomfield MA, Ashok AH, Volkow ND, Howes OD. The effects of Δ9-tetrahydrocannabinol on the dopamine system. Nature. 2016; 539(7629):369-77. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5123717/pdf/emss-70462.pdf
Blum K, Thanos PK, Oscar-Berman M, Febo M, Baron D, Badgaiyan RD, Gardner E, Demetrovics Z, Fahlke C, Haberstick BC, Dushaj K, Gold MS. Dopamine in the Brain: Hypothesizing Surfeit or Deficit Links to Reward and Addiction. J Reward Defic Syndr. 2015;1(3):95-104. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4936401/pdf/nihms-748853.pdf
Bohnert KM, Ilgen MA, McCarthy JF, Ignacio RV, Blow FC, Katz IR. Addiction. Tobacco use disorder and the risk of suicide mortality. 2014;109(1):155-62. https://deepblue.lib.umich.edu/bitstream/handle/2027.42/102156/add12381.pdf?sequence=1&is Allowed=y
Borges G, Bagge CL, Orozco R. A literature review and meta-analyses of cannabis use and suicidality. J Affect Disord. 2016;195:63-74. https://www.sciencedirect.com/science/article/abs/pii/S0165032715310004?via%3Dihub
Centers for Disease Control (CDC), Morbidity and Mortality Weekly Report (MMWR) July 24, 2015. Notes from the Field: Death Following Ingestion of an Edible Marijuana Product —
Colorado, March 2014. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6428a6.htm
Centers for Disease Control (CDC), Youth Risk Behavior Survey, Trends in the Prevalence of
Tobacco Use National YRBS: 1991—2019.
https://www.cdc.gov/healthyyouth/data/yrbs/factsheets/2019_tobacco_trend_yrbs.htm
Clarke MC, Coughlan H, Harley M, Connor D, Power E, Lynch F, et al. The impact of
adolescent cannabis use, mood disorder and lack of education on attempted suicide in young
adulthood. World Psychiatry. 2014; 13(3):322-323.
https://europepmc.org/backend/ptpmcrender.fcgi?accid=PMC4219077&blobtype=pdf
Curtin SC, Warner M, Hedegaard H: Suicide rates for females and males by race and ethnicity:
United States, 1999 and 2014 (NCHSE-Stats). Hyattsville, Md, Centers for Disease Control and Prevention, National Center for Health Statistics, April 2016.
https://www.cdc.gov/nchs/data/hestat/suicide/rates_1999_2014.htm
Dowd M. Don’t harsh our mellow dude. New York Times June 3, 2014
http://www.nytimes.com/2014/06/04/opinion/dowd-dont-harsh-our-mellow-dude.html
Evins AE, Korhonen T, Kinnunen TH, Kaprio J. Prospective association between tobacco
smoking and death by suicide: a competing risks hazard analysis in a large twin cohort with 35-
year follow-up. Psychol Med. 2017;47(12):2143-2154.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5551385/pdf/S0033291717000587a.pdf
Gex CR, Narring F, Ferron C, Michaud P. Suicide attempts among adolescents in Switzerland:
Prevalence, associated factors and comorbidity. Acta Psychiatrica Scandinavica, 1998;98(1):28-
33.
https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1600-0447.1998.tb10038.x
Gobbi G, Atkin T, Zytynski T, Wang S, Askari S, Boruff J, Ware M, Marmorstein N, Cipriani A, Dendukuri N, Mayo N. JAMA Psychiatry. Association of Cannabis Use in Adolescence and Risk
of Depression, Anxiety, and Suicidality in Young Adulthood: A Systematic Review and Metaanalysis. 2019;76(4):426-434.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6450286/
Gorelick DA, Goodwin RS, Schwilke E, Schwope DM, Darwin WD, Kelly DL, et al.
Antagonist-elicited cannabis withdrawal in humans. J Clin Psychopharmacol. 2011; 31(5):603-
12.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3717344/pdf/nihms486934.pdf
Hawton K, Casañas I Comabella C, Haw C, Saunders K. Risk factors for suicide in individuals
with depression: a systematic review. J Affect Disord. 2013;147(1-3):17-28.
https://pubmed.ncbi.nlm.nih.gov/23411024/
Kahn GD, Wilcox HC. Marijuana use ss associated with suicidal ideation and
behavior among US adolescents at rates similar to tobacco and alcohol. Arch Suicide Res. 2020;
Aug 11, online ahead of print
https://www.tandfonline.com/doi/full/10.1080/13811118.2020.1804025
Kaplan MS, McFarland BH, Huguet N, Conner K, Caetano R, Giesbrecht N, Nolte KB. Acute
alcohol intoxication and suicide: a gender-stratified analysis of the National Violent Death
Reporting System. Inj Prev. 2013;19(1):38-43.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3760342/pdf/nihms-505996.pdf
Kassel JD, Evatt DP, Greenstein JE, Wardle MC, Yates MC, Veilleux JC. The acute effects of
nicotine on positive and negative affect in adolescent smokers. J Abnorm Psychol.
2007;116(3):543-53.
https://core.ac.uk/download/pdf/192589689.pdf
Koppel BS, Brust JC, Fife T, Bronstein J, Youssof S, Gronseth G, et al. Systematic review:
Efficacy and safety of medical marijuana in selected neurologic disorders Report of the
Guideline Development Subcommittee of the American Academy of Neurology. Neurology.
2014; 82(17):1556-63.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4011465/pdf/NEUROLOGY2013552075.pdf
Langford RM, Mares J, Novotna A, Vachova M, Novakova I, Notcutt W, Ratcliffe S. A doubleblind, randomized, placebo-controlled, parallel-group study of THC/CBD oromucosal spray in
combination with the existing treatment regimen, in the relief of central neuropathic pain in
patients with multiple sclerosis. J Neurol. 2013;260(4):984-97.
https://www.researchgate.net/profile/Stuart_Ratcliffe/publication/233770159_A_doubleblind_randomized_placebo-controlled_parallelgroup_study_of_THCCBD_oromucosal_spray_in_combination_with_the_existing_treatment_re
gimen_in_the_relief_of_central_neuropathic_pain_in_patients_wi/links/57d8111a08ae6399a399
12da/A-double-blind-randomized-placebo-controlled-parallel-group-study-of-THC-CBDoromucosal-spray-in-combination-with-the-existing-treatment-regimen-in-the-relief-of-centralneuropathic-pain-in-patien.pdf
Marco CA, Detherage JP, LaFountain A, Hannah M, Anderson J, Rhee R, Ziegman J, Mann D.
The perils of recreational marijuana use: relationships with mental health among emergency
department patients. J Am College Emergency Physicians Open, January 21, 2020. Online ahead
of print.
https://onlinelibrary.wiley.com/doi/epdf/10.1002/emp2.12025
McHugh CM, Corderoy A, Ryan CJ, Hickie IB, Large MM. Association between suicidal
ideation and suicide: meta-analyses of odds ratios, sensitivity, specificity and positive predictive
value. BJPsych Open. 2019;5(2):e1.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6401538/pdf/S2056472418000881a.pdf
Miller CL. The Impact of Marijuana on Mental Health, in: Contemporary Health Issues on
Marijuana (K.Winters and K. Sabet, eds.) Oxford University Press, 2018.
https://global.oup.com/academic/product/contemporary-health-issues-on-marijuana9780190263072?q=Contemporary%20Health%20Issues%20on%20Marijuana&lang=en&cc=us
Miller CL, Jackson MC, Sabet K. Marijuana and Suicide: Case-control Studies, Population Data,
and Potential Neurochemical Mechanisms, in: Cannabis in Medicine. An Evidence Based
Approach (K Finn, ed.) Springer Press 2020.
https://www.springer.com/fr/book/9783030459673?gclid=EAIaIQobChMIrp_0wfjR6QIVSY2F
Ch1xfA-ZEAEYASABEgJuX_D_BwE#aboutAuthors
Miller M, Borges G, Orozco R, Mukamal K, Rimm EB, Benjet C, Medina-Mora ME. Exposure
to alcohol, drugs and tobacco and the risk of subsequent suicidality: findings from the Mexican
Adolescent Mental Health Survey.Drug Alcohol Depend. 2011;113(2-3):110-7
https://www.sciencedirect.com/science/article/abs/pii/S0376871610002620?via%3Dihub
Nordström P, Asberg M, Aberg-Wistedt A, Nordin C. Attempted suicide predicts suicide risk in
mood disorders. Acta Psychiatr Scand. 1995;92(5):345-50.
https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1600-
0447.1995.tb09595.x?sid=nlm%3Apubmed
Nussbaum A, Thurstone C, Binswanger I. Am J Psychiatry. Medical marijuana use and suicide
attempt in a patient with major depressive disorder.2011;168(8):778-81.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5242320/pdf/nihms841724.pdf
Olfson M, Weissman MM, Leon AC, Sheehan DV, Farber L. Suicidal ideation in primary care.
J Gen Intern Med. 1996 Aug;11(8):447-53.
https://pubmed.ncbi.nlm.nih.gov/8872781/
Pandey GN. Biological basis of suicide and suicidal behavior. Bipolar Disord. 2013;15(5):524-
41.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3749837/pdf/nihms-476618.pdf
Patton GC, Coffey C, Carlin JB, Sawyer SM, Lynskey M. Reverse gateways? Frequent cannabis
use as a predictor of tobacco initiation and nicotine dependence. Addiction. 2005;100(10):1518-
25.
https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1360-0443.2005.01220.x?sid=nlm%3Apubmed
Price C, Hemmingsson T, Lewis G, Zammit S, Allebeck P. Cannabis and suicide: longitudinal
study. Br J Psychiatry. 2009;195(6):492-7.
https://pubmed.ncbi.nlm.nih.gov/19949196/
Raja M, Azzoni A. Suicidal ideation induced by episodic cannabis use.
Case Rep Med. 2009;2009:321456.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2729295/pdf/CRM2009-321456.pdf
Randall JR, Walld R, Finlayson G, Sareen J, Martens PJ, Bolton JM. Acute risk of suicide and
suicide attempts associated with recent diagnosis of mental disorders: a population-based,
propensity score-matched analysis. Can J Psychiatry. 2014 Oct;59(10):531-8.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4197787/pdf/cjp-2014-vol59-october-531-
538.pdf
Rasic D, Weerasinghe S, Asbridge M, Langille DB. Longitudinal associations of cannabis and
illicit drug use with depression, suicidal ideation and suicidal attempts among Nova Scotia high
school students. Drug and Alcohol Dependence, 2013;129(1-2):49-53.
https://www.sciencedirect.com/science/article/abs/pii/S0376871612003730?via%3Dihub
Roberts M. Luke Goodman Killed Himself in Keystone Because of Pot Edibles, Family Says.
Westword, March 26, 2015.
https://www.westword.com/news/luke-goodman-killed-himself-in-keystone-because-of-potedibles-family-says-6616258
Roberts M. Daniel Juarez’s Stabbing Suicide Latest Death Linked to Marijuana Intoxication.
Westword, May 19, 2015.
https://www.westword.com/news/daniel-juarezs-stabbing-suicide-latest-death-linked-tomarijuana-intoxication-6727165
Russo M, Rifici C, Sessa E, D’Aleo G, Bramanti P, Calabrò RS. Sativex-induced
neurobehavioral effects: causal or concausal? A practical advice! Daru. 2015; 23(1):25.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4407789/pdf/40199_2015_Article_109.pdf
Schauer GL, Peters EN. Correlates and trends in youth co-use of marijuana and tobacco in the
United States, 2005–2014. Drug Alcohol Dependence. 2018; 185:238-244.
https://dl.uswr.ac.ir/bitstream/Hannan/49985/1/2018%20DAD%20Volume%20185%20April%2
0%2817%29.pdf
Sellers CM, Diaz-Valdes Iriarte A, Wyman Battalen A, O’Brien KHM. Alcohol and marijuana
use as daily predictors of suicide ideation and attempts among adolescents prior to psychiatric
hospitalization. Psychiatry Res. 2019;273:672-677.
https://www.sciencedirect.com/science/article/abs/pii/S0165178118323321?via%3Dihub
Silins E, Horwood LJ, Patton GC, Fergusson DM, Olsson CA, Hutchinson DM, et al. Young
adult sequelae of adolescent cannabis use: an integrative analysis. Lancet Psychiatry. 2014;
1(4):286-93.
https://www.thelancet.com/journals/lanpsy/article/PIIS2215-0366(14)70307-4/fulltext
Turner HA, Finkelhor D, Shattuck A, Hamby S. Recent victimization exposure and suicidal
ideation in adolescents. Arch Pediatr Adolesc Med. 2012;166(12):1149-54.
https://jamanetwork.com/journals/jamapediatrics/articlepdf/1384983/poa120051_1149_1154.pdf
van Reekum R, Streiner DL, Conn DK. Applying Bradford Hill’s criteria for causation to
neuropsychiatry: challenges and opportunities. J Neuropsychiatry Clin Neurosci.
2001;13(3):318-25.
https://neuro.psychiatryonline.org/doi/pdf/10.1176/jnp.13.3.318
Vijayakumar L, Michael R Phillips, Morton M Silverman, David Gunnell, Vladimir Carli
Vikram Patel, Dan Chisholm, Tarun Dua, et al. Suicide. In: Mental, Neurological, and Substance
Use Disorders: Disease Control Priorities, Third Edition (Volume 4). Washington (DC): The
International Bank for Reconstruction and Development / The World Bank; 2016 Mar 14.
Chapter 9.
https://www.ncbi.nlm.nih.gov/books/NBK361942/?report=printable
WHO, Global Report on Trends in Prevalence of Tobacco Use, 2000-2025, Third Edition, 2019.
https://apps.who.int/iris/bitstream/handle/10665/330221/9789240000032-eng.pdf
Zammit S, Allebeck P, Andreasson S, Lundberg I, Lewis G. Self reported cannabis use as a risk
factor for schizophrenia in Swedish conscripts of 1969: historical cohort study. BMJ.
2002;325(7374):1199.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC135490/pdf/1199.pdf
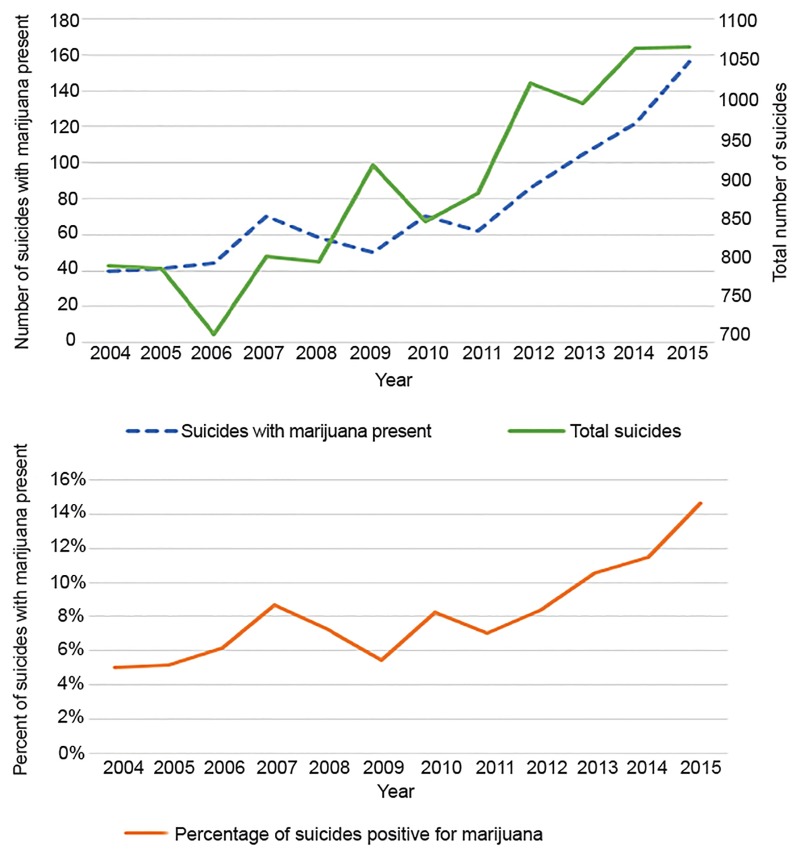
Legalized Cannabis in Colorado Emergency Departments: A Cautionary Review of Negative Health and Safety Effects
Brad A. Roberts, MD
In the most recent data on Colorado adolescent suicides, marijuana was the most common substance present for ages 10–19 in 2016. Of 62 suicides with toxicology data available, marijuana was present in 30.6% (n = 19) compared to 9.7% (n = 6) for alcohol.24 This trend has been increasing since liberalization of marijuana policy in 2010. This is more concerning as suicide is currently the leading cause of death of adolescents in Colorado.25 For all age groups in Colorado, in the five-year period from 2004–2009 there were 4822 suicides and 7.1% (n = 303) of those were marijuana positive on toxicology analysis (538 did not have toxicology data available). In the subsequent five-year period of marijuana legalization, 2010–2015, there were 5880 total suicides (22% increase), and 12.6% had a positive toxicology for marijuana (n = 601; 1,120 did not have toxicology data available). This represents a statistically significant 77.5% increase in the proportion of suicide victims with toxicology positive for marijuana (an absolute difference of 5.5%) for which toxicology data were reported (chi square 77.2884, p<0.0001). Suicides with marijuana toxicology by year and overall suicide by year data are displayed
in Figure 5.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6625695/
Evaluation of State Cannabis Laws and Rates of Self-harm and Assault
Question Are state cannabis legalization laws with varying degrees of commercialization associated with rates of self-harm or assault injuries?
Findings In this cohort study based on health insurance claims data from 75 395 344 beneficiaries between 2003 and 2017, rates of self-harm injuries among males younger than 40 years increased more in states legalizing recreational cannabis dispensaries compared with states without cannabis legalization laws. For other age and sex groups and for more restrictive legalization approaches, no association with self-harm and assault was found.
Meaning States with recreational cannabis may benefit from monitoring levels of self-harm as a potential consequence of legalization.
https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2777634